Man's eyes are not only a “mirror of the soul”, but also an important organ of feelings. Deviations in the work of the visual apparatus can provoke not only visual impairment, but also a violation of the overall well -being of a person. An important criterion characterizing the health of the eyes is an indicator of eye pressure. The deviation of the value of ophthalmotonus both towards the increase and in the direction of decrease is a violation and requires an additional examination of the patient. What indicators are the norm of eye pressure in women and men? What corrective measures will help normalize ophthalmotonus?
Content
- What is eye pressure
- How to measure eye pressure
- Eye pressure in adults - indicators of the norm and options for deviations
- Eye pressure - diagnostics at home
- Glaucoma and eye pressure
- How to treat increased eye pressure drugs
- Reduced eye pressure - drug treatment of violation
- Eye pressure - folk methods of correction of deviations
- How to relieve eye pressure - therapeutic gymnastics for the eyes
What is eye pressure
The wording of the “eye bottom pressure” (ophthalmotonus) characterizes the degree of voltage between the contents of the eyeball and its shell. This parameter determines the pressure that the vitreous body and the eye fluid on the walls of the eyeball, the cornea and the sclerus. Every minute in the eye there is an flow and outflow of about 2 cubic meters. mm fluid. When the balance of the influx and the release of the liquid is observed, normal ophthalmotonus is observed. Violation of this process leads to an increase or decrease in eye pressure. Both states are hazardous to health and require correction.
Type 3 types of ophthalmotonus are distinguished:
- Transient - characterized by a short -term change in the indicator and further return to the boundaries of the norm.
- Laby - also the pressure also changes temporarily with subsequent normalization, but such changes occur regularly.
- Stable increased pressure is constant, due to which it is the greatest danger to humans.
Eye pressure - causes of deviations
An increase and decrease in ophthalmotonus can cause various causes - these are the patient’s age, and the presence of chronic diseases, as well as surgical interventions (especially eyes). An additional risk of deviations in the indicators of eye pressure is observed in people suffering from diabetes mellitus, cardiovascular pathologies with eye diseases, farsightedness and hereditary predisposition to the disease. High eye pressure occurs more often than lowered.
Reasons for increasing ophthalmotonus:
- Functional disorders in the body, the result of which is enhanced fluid production.
- Deviations in the work of the cardiovascular system.
- Strong stress.
- Increased physical activity.
- Excessive enthusiasm for coffee.
- Frequent alcohol consumption.
- Strong cough, bouts of vomiting.

Causes of low ophthalmotonus:
- Increased eyes voltage caused by long -term work at the computer, reading in poor light, etc.
- Inflammatory processes that affect the vascular mesh of the eye shell.
- Camping eye injuries leading to the appearance of fistulas (holes), entering the eye of foreign bodies.
- Metting of the retina.
- Reduced blood pressure.
- Dehydration.

Eye pressure - symptoms of increased and reduced ophthalmotonus
With an increase and with a decrease in the eye pressure, the manifestation of the disease will be different. Moreover, symptoms in men and women also have its own characteristics.
With increased ophthalmotonus, complaints about:
- Headaches in the temples.
- Dizziness.
- Soreness in the eyes.
- Discomfort when lifting eyebrows.
- Reducing the field of visibility (latitude of lateral vision).
- Veasure of vision at dusk and in poor light.
- Filling out vision, especially immediately after awakening.
- A pronounced vascular mesh in front of our eyes, bursting capillaries.

With hypotension, the eyes are often noted such symptoms as:
- Dryness and discomfort in the eyes (frequent blinking).
- Loss of a characteristic shine of a moisturized surface of the eye.
- Soreness in the eye area.
- Discomfort in the form of pop -up points, periodic burning and short -term clouding of vision.
- Darkening in the eyes.
- Vision of vision.
With minor deviations in the indicators of eye pressure, a person may not feel discomfort - signs of eye pressure disorders may be absent. The patient does not even realize the violations. In addition, a jump, like a drop in pressure, can be of a short -term episodic character and not talk about the need for special therapy at all. The optimal method for controlling the health of the eyes is a regular (at least 1 time per year) visit to an ophthalmologist.

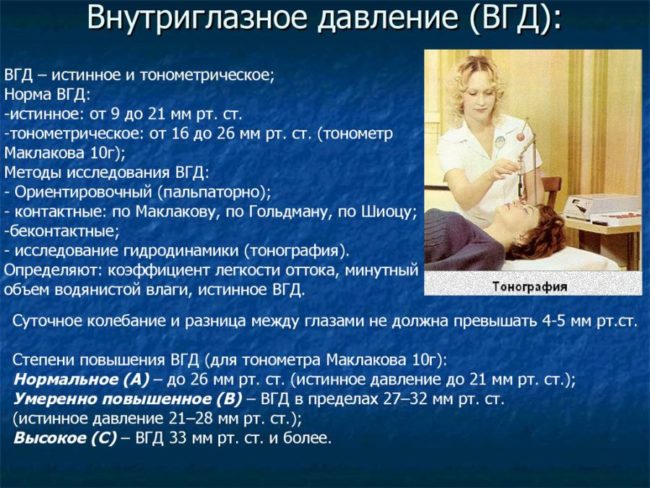
How to measure eye pressure
The measurement of eye pressure indicators is made at an ophthalmologist. In clinical practice, the following methods are most applied to measure eye pressure:
- Contact tonometry using an electronographer.
This technology is the safest. The procedure does not bring absolutely any discomfort. The technique is based on increasing the production of intraocular fluid and accelerating its outflow. The equipment is quite expensive, so it is more common in private specialized centers.
- ICARE contactless tonometer.
Expensive equipment, so not every medical institution is equipped with it. Diagnosis is carried out using a special disposable sensor. The latter is in contact with the cornea and fixes the necessary data.

- Pneumotonometry.
The center of the cornea is exposed to the air stream. The study is performed quickly and does not cause special inconvenience. The disadvantage of this method is not too high accuracy. To determine the true indicators, 4 measurements are made.
- Tonometry according to Maklakov.
The procedure is not painful, but not too pleasant. It is carried out under local anesthesia. During tonometry, a weight is placed in the center of the cornea. After its removal on the surface of the eye, a certain imprint remains. Measurements of the parameters of the resulting print allow us to draw conclusions about the patient's ophthalmotonus. The method cannot be called modern, but its diagnostic value is quite high.
If in the doctor’s arsenal there are no special devices to determine the eye pressure, the conclusion about the state of ophthalmotonus is made on the basis of a manual examination. During the palpation, the doctor presses with index fingers over the eyelids and, based on sensations, draws conclusions about the density of the eyeballs. This research method, of course, cannot be called final, but it can determine the need for a further more detailed examination.

Eye pressure in adults - indicators of the norm and options for deviations
Evaluation of these eye pressure is based on their compliance with the established criteria of the norm.
Normal eye pressure
Eye pressure indicators are normal for patients of different ages.
- The constant accepted norm is an ophthalmotonus in the range from 12 to 22 mm. RT. Art. These values \u200b\u200bare indicative for all people up to 40 years.
- The average magnitude of the eye pressure is 15 - 17 mm. RT. Art.
- During the day, eye pressure experiences small (3 - 4 mm. Rt. Moreover, the largest numbers are marked in the morning. By the evening, there is a slight decrease in indicators.
Age changes affect all human organs and systems. Eyes were no exception. Regular examinations of the fundus at the ophthalmologist become especially relevant, because the risk of glaucoma is increasing. What eye pressure is the norm in older people?
- In 50 - 60 years, normal eye pressure ranges from 23 - 25 mm. RT. Art.
- 70 years old and older than the norm is an ophthalmotonus in the interval of 23 - 26 mm. RT. Art.
These values \u200b\u200bdo not indicate the presence of pathology.
Indicators of reduced eye pressure
Hypotenia of the eye (or reduced eye pressure) is characterized by a decrease in the ophthalmotonus indicator. The situation is considered an alarming when the eye pressure drops below 10 mm mark. RT. Art. Mildly expressed hypotension of the eye may not manifest itself for a long time. Moreover, this condition is as dangerous as increasing eye pressure. Reduced ophthalmotonus is often observed in people with diabetes.
High eye pressure indicators
People are more often predisposed to increase intraocular pressure indicators, although the disease can also affect young people. The pressure provokes a weak fluid outflow. The eye hypertonicity is noted in case of an exceeding the indicator 22 mm. RT. Art. (taking into account the age of the patient).

Eye pressure - diagnostics at home
In the presence of symptoms indicating a possible decrease or increase in eye pressure, the initial diagnosis can be carried out at home. This is necessary:
- Close your eyes and place your finger on the eyelid.
- Make a light pressure on the eyeball.
- With increased ophthalmotonus, the ball will be poorly deformed and feel firm enough. In the case of hypotension of the eye, the eyeball will be unnecessarily crushed. A rounded and moderately elastic ball is an indicator of the norm.
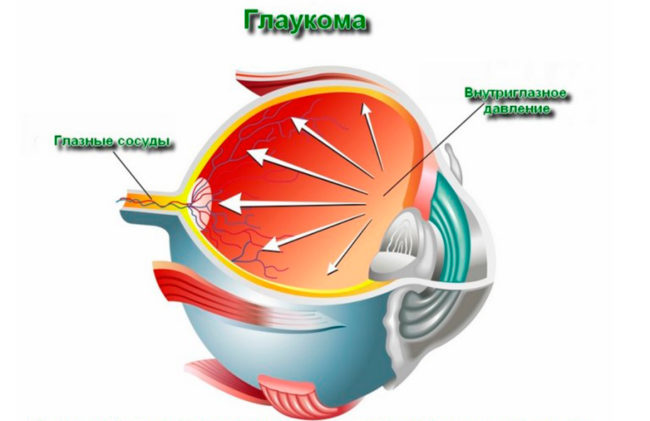
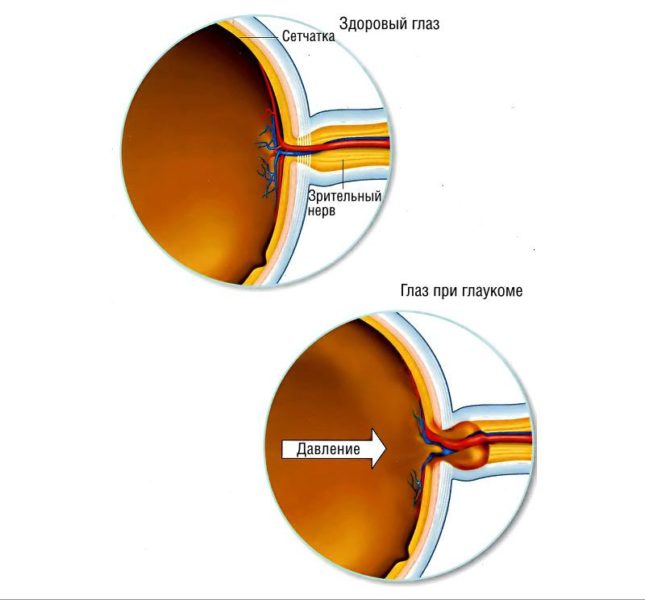
Glaucoma and eye pressure
Glaucoma is a rather dangerous eye disease. Pathology can be both congenital and acquired. The danger of the disease lies in the gradual destructive effects on the eye nerve. The lack of treatment leads to a complete and irreversible loss of vision. The lesion of the eye nerve occurs under the influence of increased eye pressure. It is impossible to ignore this condition.
- Suspicion of the development of glaucoma occurs already with stably increased indicators of eye pressure - 23 - 25 mm. RT. Art.
- The initial stage of glaucoma is not accompanied by a pronounced deviation of the ophthalmotonus indicator. In a number of cases, a slight excess is possible (by 4 - 5 mm. RT. Art.) Norms. At the beginning of the disease, the pressure usually does not exceed 27 mm. RT. Art.
- Further development of pathology leads to an increase in eye pressure. At this stage, the numbers of ophthalmotonus often fluctuate within 27 - 33 mm. RT. Art.
- When the disease has already gone far, eye pressure indicators exceed 33 mm. RT. Art. This stage of glaucoma is final.
How to treat increased eye pressure drugs
The identified systematic deviations cannot be ignored. Therapy is selected individually, taking into account the severity of the pathology, age of the patient and his general history. Complex therapy gives a good result - combinations of medications and folk remedies. With regard to the latter, it is worth mentioning - any treatment should be agreed with the doctor. In the presence of increased eye pressure, the prescribed medications are designed to improve the abduction of excess eye fluid. Additional components of drugs nourish the eyes.
The following drops from eye pressure got into this category of funds:
- Tafluprost - reduces ophthalmotonus, is used in the treatment of glaucoma;
- Xalatan - reduces intraocular pressure, improves moisture outflow;
- Grass - slows down the progression of glaucoma, helps to remove fluid;
- Trusop;
- Azop.
The first 3 drugs belong to the group of prostaglandins. Medicines are quite effective, but have a number of side effects. So prolonged use of these medications leads to a narrowing of the patient's pupil. As a result - a decrease in the field of vision, the appearance of pain in the temporal and frontal parts of the head.
Trusop and AZOP are belonging to the category of carbooangidrases. These drugs do not cause a deterioration in the condition of vision, but can negatively affect the work of the kidneys.
- Beta-blockers are called to reduce the amount of fluid released (for example, Timoptic, Betaxolol, Timolol).
- The action of M-cholinomimetics (pillycarpin) is also aimed at improving the outflow of excess fluid.
If conservative treatment does not have the desired effect, it is advisable to think about surgical intervention. A good result is shown by a lasernaya operation, during which the outflow of intraocular fluid is opened. As a result, a decrease in ophthalmotonus. However, this intervention is not allowed to everyone.

Reduced eye pressure - drug treatment of violation
In the case of hypotension, both conservative and surgical treatment are possible. The first includes:
- oxygenotherapy (treatment with oxygen);
- injection with vitamin B1;
- the appointment of drugs that gently increase intraocular pressure (for example, aloe, atropine, 1%cortisone emulsion);
- injections of dexamethasone or sodium chloride solution;
- the use of medicines aimed at eliminating vascular cramps and treatment of atrophy;
- antibacterial agents (if necessary).
It is worth noting that the above methods and types of drugs are not used simultaneously. The choice of specific treatment tactics is determined by the individual characteristics of each patient.

Eye pressure - folk methods of correction of deviations
In the case of increased ophthalmotonus, the help of meadow clover, the plants of the golden mustache are often used.
- Take 1 tbsp. l. dried clover and pour it 100 ml of boiling water. Insist a decoction of 2 hours. Strain and drink 100 ml daily before bedtime.
- 17 Kolenets of the Golden mustache fill 0.5 liters of vodka. Send the composition to insist in a dark place for 12 days, not forgetting to shake the infusion every 3 days. Take 1 tbsp before breakfast. l. (1 time per day).
- Place a pinch of cinnamon in a glass of kefir and drink the composition. Repeat the procedure daily (better before bedtime).
- 25 g of herbs, pour 500 ml of boiling water. When the decoction is infused, strain it through gauze. Make lotions from the finished product during the day.
- It will help normalize eye pressure natural tomato juice. Every day you need to drink 1 glass of product.
- 2 Potato tuber clean, wash and rub on a grater. Add 1 tsp. Apple vinegar. Mix the components and leave for 20 minutes. Put the finished slurry on gauze and apply as a compress.
With hypotonus, the eyes helps aloe well. Cut into pieces of 5 - 6 sheets of aloe. Pour raw materials with a glass of boiling water and check for another 5 minutes. Rinse your eyes with a finished decoction (3 - 5 times a day). During the manipulation, a burning sensation or other unpleasant symptoms often occur. You should not stop the procedures because of them.

How to relieve eye pressure - therapeutic gymnastics for the eyes
Performing simple exercises will not only have a good prevention of eye pressure disorders, but also help improve the condition with already emerging problems. The main goal of gymnastics for the eyes is to relieve tension and improve the blood circulation of the eye.
- Perform stroking your forehead with your palms. First, go from the middle of the forehead to the temples, and then from the eyebrows to the forehead.
- Go to the window and look through the glass outside. Choose any long -distance point and focus on it for a few seconds. And then look at the glass itself. Repeat the exercise 10 times.
- For 3 minutes, lightly tap your fingertips on the forehead.
- Perform circular massaging movements in the temples.
- Put the index finger before your eyes. Look in front of you (as if through your finger), then look at your finger and down. Repeat the exercise 15 times.
- Close your eyes and gently massage for 1 minute of the century.
- The eyes are closed. Make a light pressure on the eyelid, and then let go. The number of repetitions is 7.
- Alternately, look from left to right and vice versa.
- Rotate with your eyes first in one direction, and then in the other.
Adhere to a balanced diet, do not overwork and do not forget about moderate physical activity, and then your eyes will not remind you of anxious symptoms for a long time.










Comments
a couple of years ago, there was no side of metrogils from the same problem, there were no side effects ...
I’m not a fan of peeling at all, it saves from acne of metrogil, it also smoothes it ...
Great article! ...
I take the second course of the Capsules Climafite 911. The tides went very quickly. It became calmer, irritability went away and I sleep well ...
i also noticed - it is worth nervous, everything immediately affects the face. Therefore, I try to avoid conflicts and unpleasant people. Of the creams, I like Miaflow from wrinkles - smoothes not only small wrinkles ...